Contents
Introduction……………………………………………………………………………………………………………………………….3
Background………………………………………………………………………………………………………………………………..4
Management……………………………………………………………………………………………………………………………..5
Potential complications and post-operative education ……………………………………………………………..13
Involvement of the interdisciplinary team …………………………………………………………………………………14
Conclusion………………………………………………………………………………………………………………………………….14
References ………………………………………………………………………………………………………………………………..15
Introduction
In the given case study, we need to identify the nursing process while managing the wound management and the medical history of the patient (Ackley, 2018). We would be further evaluating the discussion around the nursing management and would also create an analysis related to patient post-surgery. There would be careful in general and would further interpret prioritized nursing diagnosis/ problems.
The nursing process is one of the systematic and scientific approaches that help in managing a range of patients. Through this report, we would be understanding how the nursing process can help in while taking care of the post-surgery patients that have been admitted.
The nursing process involves a healing process and is used as a tool to provide a quality of patient care. The nursing process has essential steps such as the assessment, diagnosis, planning, implementation, evaluation.
Background
|
Identify |
Fall from the bicycle during the marathon, transported through ambulance to ED |
|
Situation |
Josie has a pain in the right lower leg, resulting in the deformity, gradually leading to the swelling, and a 10cm lacerated wound. Under the observations checked the T-36.4oC, HR-90bpm, RR-22pm along with the BP-136/72mmHg, O2-95% RA, and pain score 10/10 on movement (Cabaço, 018).
|
|
Observations |
Josie has shown reactions to the Penicillin along with the oral contraceptive pill, but so far no problems. |
|
Background |
Josie needs to have an opioid analgesia during the ED. From the x-ray shows the fracture within the Right tibia and fibula. Subsequently the orthopedic team, did a quick operation upon the surgery in order to reduce the open reduction along with the internal fixation (ORIF) with respect to the fracture.
|
|
Agreed Plan |
The patient as such returned from the 12.30 hrs post-op orders as per the routine observations, wound dressing which needs to be for 72hrs. Also additionally there needs to be a bung IVT placed with the current bag completed and also a neurovascular observations within the two-hourly duing the first 48-hours, and also need to put on non-weight having crutches. So far the condition is drowsy but alert to voice; and also has a dressing upon her right lower leg requiring a minimal sanguineous ooze evident. The condition is: T-35.5oC, HR-66bpm, RR-16pm, BP-109/71mmHg, O2-97% via HM at 6LPM, and pain score 2/10. Given a quick prophylactic Ceftriaxone 2g IV during surgery. Also anesthetist has given the medication of Paracetamol 1g IV/PO 6 hourly, Ibuprofen 400mg PO TDS, Tramadol SR 100mg PO BD prn, and Ceftriaxone 2g IV/ IM 6 hourly for 2 further doses. IV Compound Sodium Lactate 1L which is at six-hourly rate with respect to the Josie's left arm. |
|
Read Back |
Need to provide timely medication and monitor the patient current condition. |
Management
To provide quality care to the post-surgery patient, the nurses need to follow an evidence-based practice. In the postoperative surgery, it helps the nurses to identify and address problems which are related to the individual patient. It is important as a nursing student to understand the preoperative condition of the patient and apply suitable nursing process (Butcher, 2018). There should be a comprehensive plan of care, which would be based on the assessment along with the focus on the outcomes which would help in the improved care and the reduced pain. The main aim is to help women patient have a faster recovery from the given major surgery. There should also be a progressive goal associated that would provide nursing care with respect to the patients which can help in achieving the procedure to be evaluated. Through this report, we would be understanding the nursing process and would also help in delivering nursing care to the patients.
Assessment of Data
Subjective Data
Complain of pain in the patient right lower leg, causing a deformity along with the significant swelling (Caldeira, 2016). A surgery for open reduction and internal fixation (ORIF) of the fracture. It has been observed from the post-op orders to check the routine observations wound dressing in order to keep the 72hrs and also making the bung IVT to check the neurovascular observations. Current condition is drowsy but alert and responsive to voice. So far dressing on the right lower leg, with minimal sanguineous ooze evident.
Objective
The vital signs of the patient is T-36.4oC, HR-90bpm, RR-22pm, BP-136/72mmHg, O2-95% RA, and pain score 10/10 on movement opioid analgesia in ED for her pain and X-ray confirms the diagnosis of the open fracture of the Right tibia and fibula. The patient requires a right leg surgery with wound dressing (D’Agostino, 2016). From the brief evaluation of the patient post operative surgery, the patient Also the patient was given prophylactic Ceftriaxone 2g IV during surgery. The anesthetist has prescribed Paracetamol 1g IV/PO 6 hourly, Ibuprofen 400mg PO TDS, Tramadol SR 100mg PO BD prn, and Ceftriaxone 2g IV/ IM 6 hourly for 2 further doses. IV Compound Sodium Lactate 1L is running at a six-hourly rate into Josie's left arm.
Assessment Tools
The assessment would be done on the affected leg injury, muscle movement and the post operative surgery tools and techniques.
Fall Risk
The fall risk measured is less than 10 hence the patient is at lower risk. The condition of the patient is stable and requires routine monitoring (De Oliveira, 2016). Through this tool, we w=have evaluated the patient condition and the postoperative discharge status.
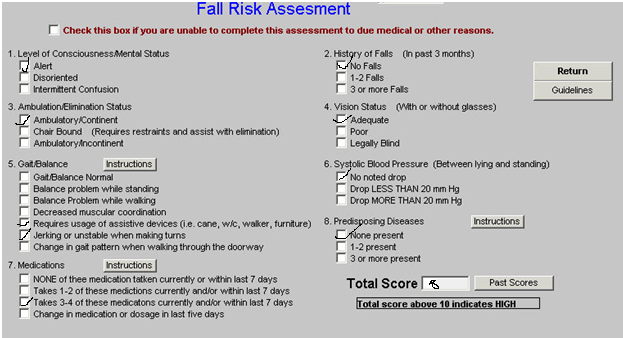
Source : (Ackley, 2016)
Braden Scale
The patient health is stable but on assessment total points possible is 23 but the patient has scored 16 or less. This means that the patient is in a moderate risk zone (Doenges, 2016).
Braden Scale scores rated below-:
1 = Highly Impaired
3 to 4= moderate or low impairment
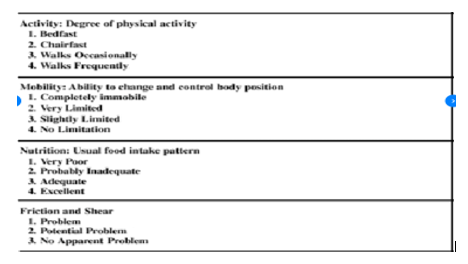
Source : (D’Agostino, 2016)
Pain Assessment
Source : (D’Agostino, 2016)
The pain assessment shows that the patient is currently at pain, but her condition is not very volatile or at high risk. The patient is adapting and currently looks stable in improving medical conditions (Frauenfelder, 2016).
- Nursing diagnosis –
The nursing diagnosis needs to be evaluated with the help of the below DIEP parameters such as-
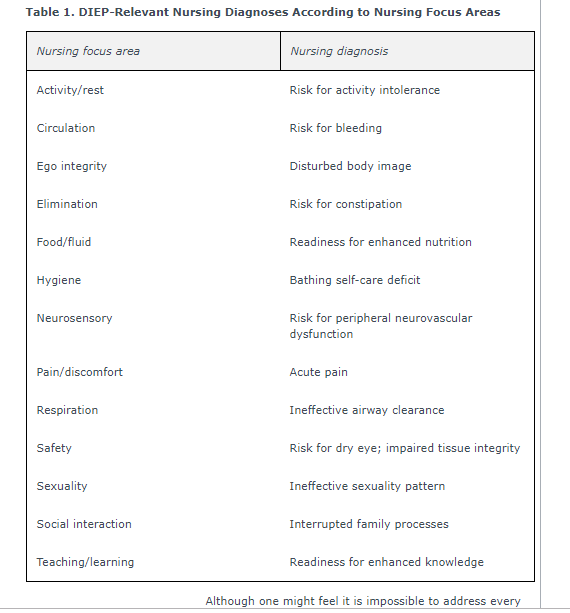
Source : (D’Agostino, 2016)
To interpret the priority below diagnosis was done through primary survey
Source : (Ackley, 2016)
Activities of daily livings
The activities daily livings affected would be
Routine bathroom activities
Restricted move ability from one place to another
Limited leisure activities (Potter, 2016).
Nursing Diagnosis of hypothermia post surgery is a risky condition under which there is a medical emergency which can occur inside the body which leads to loss of the heat faster with respect to producing the heat, resulting in the low body temperature. The condition of the hypothermia normally occurs when the body temperature falls below 95 F (35 C)
Planning
Planning-
Prioritized plans such as hypothermia post surgery would be done like below
To have a specific planning, we need to constantly check with the thermohygrometer which would be done every 20 minutes, after which keeping body warm and regulating the room temperature. To check the measurability, we need to constantly measure the patient sensitivity, and understand the movements of the legs movement along with checking if the patient has overcome the anesthetic agent actions. It can be achieved through the specific medication along with the constant care and finally by constant monitoring (Menna Barreto, 2016). Such measurements and planning are realistic which can be achieved through the constant monitoring of body temperature, medication along with the proper timely care It would take a time Frameof 2 days and the other goals within 2 weeks to achieve the applied goals.
The implementation would include the following method
It would done through the constant nursing interventions, documentation along with the referral to a multidisciplinary team such as the anesthesia team, orthopedic team, and doctor alertness. Such applied and implemented methods are measurable as it can be measured through the patient improvement along with the responsiveness to medication and finally through the increased resistance to the pain and having medication. It can be achieved through the medication, constant care along with the constant regulation of body temperature. It can be realistically achieved with constant monitoring of body, regulation of room temperature & medication. It can be achieved within the time frame of the 2 days and the other goals within 2 weeks (Orthwein, 2017).
- Evaluation
In order to evaluate the patient condition, it was important to have an implementation plan and nursing interventions. It is expected to provide several health benefits.
2nd nursing diagnosis is
Risk of bleeding post operatively -: Bleeding can be one of the postoperative mortality which can be reviewed post operative surgery. To understand nursing intervention, it is important to understand the blood loss and the required anticoagulant medications that can help in preventing the condition of the thromboembolism. Post operative surgery can lead to the severe bleeding risks and there are a numerous clinical factors which are associated with the increased risk of hemorrhage or other related impact.
Planning-
Prioritized plans such as risk bleeding post operatively would be done like below
To understand the specific outcomes we need to understand the oxygen levels are back to normal every hour , communicating with the team of experts and check if the vital signs are stable. Such outcomes are measurable through the patient sensitivity, through the team of doctors assessment and even checking if the patient has stabilized vital signs. It can be achieved through medication, constant care and even through constant monitoring. It can be realistically achieved with constant monitoring of vital signs such as BP, by giving medication & finally through the timely intervention and communicating with team of doctors. It can be achieved within the time frame of the 2 days.
The implementation would be applied through the below procedure-:
It can be achieved through the nursing interventions, documentation and finally through the monitoring condition by the multidisciplinary team such as the anesthesia team, orthopedic team, and doctor alertness. It can be measured through the patient improvement, responsiveness to medication and increased resistance to the pain and having medication. It can be achieved through medication, constant care and stabilizing of the vital signs. It can be realistically achieved with constant monitoring of body, team of doctors communication & medication. It can be achieved within the time frame of the 2 days or take a 1 weeks of time (Orthwein, 2017).
- Evaluation
To determine the patient current condition and evaluate the condition of the risk of bleeding.
The third nursing diagnosis is the respiratory depression as follows-:
The planning process includes the nursing interventions, documentation, referral to a multidisciplinary team such as the anesthesia team, orthopedic team, and doctor alertness. It can be measured through the patient improvement and responsiveness to medication, increased resistance to the pain and having medication. It can be achieved through medication, constant care and even through physiotherapist lessons. It can be realistically achieved with constant monitoring of and supervision. It can be achieved within the time frame of the 4 weeks and the other goals within 3 months (Orthwein, 2017).
To check the Implementation part of the respiratory depression is as follows-:
It needs to be specifically should be in control the problem of respiratory depression by monitoring and checking. Can be measured by the ABG and other interventions and can be achieved by the Patient airway and by providing supplemental oxygen and needs to be realistically be achieved and controlled within 24-48 hours of time frame and needs to be restored per the restore normalcy within week or months.
Evaluation
The specific goals are to evaluate and consider the result on account of the interventions (Park, 2016). It involves the reduced inflammation within the short timeframe; and even there is increased drowsiness due to the surgery, right leg pain and sensitivity to the movement. It needs to be controlled with the overall recovery.
Potential complications and post-operative education
The preoperative condition of the patient was unstable and was also complicated with the severe complications that the nurse and patient should be aware of (Potter, 2016).
The patient and the nurse needs to understand post-operative education. There is related to the direct, high pain which involves the consequences such as the narcotics required with the immobility, and also involved with the lengthy post-operative recovery period.
This tends to also include fail that are also related to identifying the relevant nursing diagnoses with respect to the patients (Silva, 2017). There needs to be fewer resources which can relate to the problems that can simplify the complex surgery. This tends to also help in tackling the comprehensive discussion around the diagnoses and also have a potential intervention, With the help of identified nursing diagnosis, it would help in more explicit or slow down process which can help in providing an effective process of the interventions to promote healing.
The postoperative surgery education to be provided to the patient is to restrain from creating pressure on the right leg, avoid walking from that foot unless there are signs of improvement and constantly have a good diet, nutrition and do physiotherapy exercises. Apart from this, it is also important to adhere to the medication and avoid any sort of stress. In the case of increased pain sensation or any troubles, the patient needs to touch base with the doctors and the teams (Silva, 2017).
Involvement of the interdisciplinary team
The involvement of the orthopedic doctor was to identify pain, jerks and postoperative surgery status of the right leg. The X-ray department needs to check if there has been bone recovery. The anesthesia department has to timely check the dosage and the post-condition of the patient. The nursing department has to timely monitor the patient condition and accesses the important vital conditions of the patient. It needs to also ensure that the patient is recovering and the physician is timely checking the health of the patient (Wilson, 2017). The nurse needs to understand the patient's health, the pre, and post condition of the patient and take appropriate care of the patient. As a nursing student, it is also important to identify and evaluate applicable nursing diagnoses and match with the relevant outcome identification, care planning along with the implementation processes in order to achieve the desired outcomes.
Conclusion
Through this report, the nursing process was accessed along with the adequate diagnosis and the monitoring conditions (Wilson, 2016). Subsequently, the nursing process needs to be checked on the five parameters such as the assessment, Diagnosis, Planning, Implementation, and Evaluation. Also, the nursing diagnosis and the challenges were identified which were checked through the SMART goals. It was established that the patient who fell from the bicycle in marathon had a pain in the lower leg, which had an obvious deformity, significant swelling, and a 10cm lacerated wound. After which the open fracture identified on the Right tibia and fibula leading to the surgery in order to reduce the open reduction along with the internal fixation (ORIF) with respect fracture. This requires post-surgery routine observations need to be done to check the wound dressing.
References
Ackley, B. J., Ladwig, G. B., Msn, R. N., Makic, M. B. F., Martinez-Kratz, M., & Zanotti, M. (2019). Nursing Diagnosis Handbook E-Book: An Evidence-Based Guide to Planning Care. Mosby.
Butcher, H. K., Bulechek, G. M., Dochterman, J. M. M., & Wagner, C. (2018). Nursing Interventions Classification (NIC)-E-Book. Elsevier Health Sciences.
Cabaço, S. R., Caldeira, S., Vieira, M., & Rodgers, B. (2018). Spiritual coping: A focus of new nursing diagnoses. International journal of nursing knowledge, 29(3), 156-164.
Caldeira, S., Timmins, F., de Carvalho, E. C., & Vieira, M. (2017). Clinical validation of the nursing diagnosis spiritual distress in cancer patients undergoing chemotherapy. International journal of nursing knowledge, 28(1), 44-52.
Caldeira, S., Timmins, F., de Carvalho, E. C., & Vieira, M. (2016). Nursing Diagnosis of “Spiritual Distress” in women with breast cancer: prevalence and major defining characteristics. Cancer Nursing, 39(4), 321-327.
D’Agostino, F., Vellone, E., Cerro, E., Di Sarra, L., Juárez-Vela, R., Ghezzi, V., ... & Alvaro, R. (2016). Psychometric evaluation of the Positions on Nursing Diagnosis scale. Applied Nursing Research, 29, e1-e6.
De Oliveira, M. R., Da Silva, V. M., Guedes, N. G., & de Oliveira Lopes, M. V. (2016). Clinical validation of the “sedentary lifestyle” nursing diagnosis in secondary school students. The Journal of School Nursing, 32(3), 186-194.
Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2016). Nursing diagnosis manual: Planning, individualizing, and documenting client care. FA Davis.
Frauenfelder, F., van Achterberg, T., Needham, I., & Müller Staub, M. (2016). Nursing diagnoses in inpatient psychiatry. International journal of nursing knowledge, 27(1), 24-34.
Mangueira, S. D. O., & Lopes, M. V. D. O. (2016). Clinical validation of the nursing diagnosis of dysfunctional family processes related to alcoholism. Journal of advanced nursing, 72(10), 2401-2412.
Marques-Vieira, C. M. A., Sousa, L. M. M. D., Carias, J. F. D. M. M., & Caldeira, S. M. A. (2015). Nursing diagnosis" impaired walking" in elderly patients: integrative literature review. Revista gaucha de enfermagem, 36(1), 104-111.
Menna Barreto, L. N., Swanson, E. A., & de Abreu Almeida, M. (2016). Nursing outcomes for the diagnosis of impaired tissue integrity (00044) in adults with a pressure ulcer. International journal of nursing knowledge, 27(2), 104-110.
Orthwein, W. C. (2017). Psychiatric and mental health nursing: The craft of caring. CRC Press.
Park, H. S., Cho, H., & Kim, H. S. (2016). Development of an evidence-based nursing process system to improve clinical decision Making with colorectal cancer nursing diagnosis. Journal of Korea Multimedia Society, 19(7), 1197-1207.
Potter, P. A., Perry, A. G., Stockert, P., & Hall, A. (2016). Fundamentals of Nursing-E-Book. Elsevier Health Sciences.
Sanson, G., Alvaro, R., Cocchieri, A., Vellone, E., Welton, J., Maurice, M., ... & D'Agostino, F. (2019). Nursing diagnoses, interventions, and activities as described by a nursing minimum data set: a prospective study in an oncology hospital setting. Cancer Nursing, 42(2), E39-E47.
Silva, O. M. (2017). Impaired Physical Mobility in Chronic Kidney Disease: Nursing Diagnosis. Nurse Care Open Acces J, 3(3), 00076.
Urden, L. D., Stacy, K. M., & Lough, M. E. (2017). Critical care nursing: diagnosis and management. Elsevier Health Sciences.
Wilson, D., & Rodgers, C. C. (2016). Wong's essentials of pediatric nursing. Elsevier Health Sciences.
