Table of contents
Proposed solution and future scope of the study. 3
Discussion of board interaction. 6
Assignment 1B: Project Problem Statement 7
Problem statement of the project 7
Primary care nursing has been considered to be an essential part of the Healthcare system. This is because primary care helps in reducing complications with the help of early intervention and prevention. However, this sector often encounters lack of choice due to different working patterns of general practitioner and nurses. Moreover, in order to promote higher quality primary care practices, several technological innovationshave been adopted thereby increasing expense of care. This is evident from the expenditure of National Health Service (NHS), which has been increasing by 3.7 % per year (Montgomery et al. 2017). Increase or growth in population is furthermore, expected to limit per capita growth to 0.1%. Along with this, the prevalence of chronic disability and non-communicable diseases has increased thereby resulting in 2.9 million victims of multiple long-term conditions as of 2018.
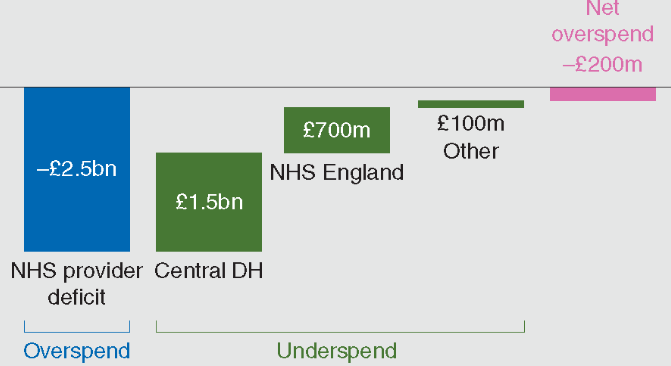
Figure 1: Spending of several primary care institutions against the Department of Health budget in terms of cash in between 2015 to 2016
(Source: Inspired from Montgomery et al. 2017, p.1751)
In between 2012 to 2013, 11% of Healthcare providers of NHS have been observed to be deficit which moreover, increased to 65% in between 2015 to 2016. Based on the ideas of Litchfield et al. (2015), these circumstances in turn, have worsened key performance matrix besides making the social Health Care integration poor. The above mentioned figure have also revealed that NHS has overspend its budget by £2.5 billion thereby indicating use of poor care models.
Proposed solution and future scope of the study
Taking the above challenges into consideration, it can be mentioned that there is requirement of adopting an effective primary care model by which fundamental appraisal of the society can be maintained. Taking ideas from Jones et al. (2016), primary care model needs to be such that supports local healthcare professionals to collaborate and improve existing care system. This improvement would be in terms of reduced cost, improved care for care seekers and better population health. This model would reconcile “top-down” and “bottom-up” approaches.
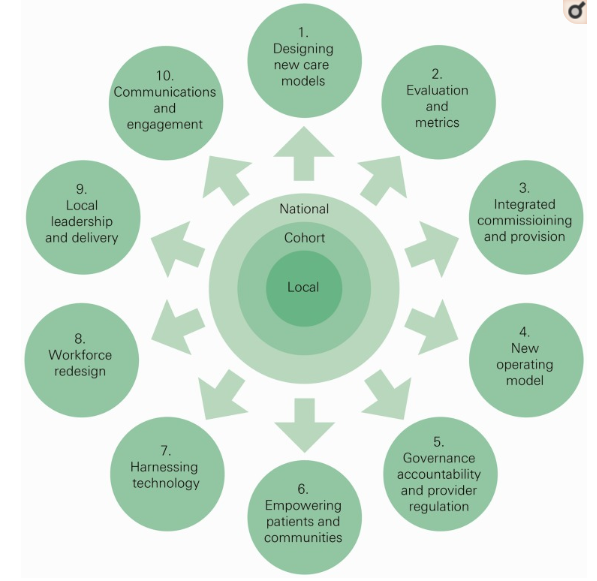
Figure 1: Features of the new model of care
(Source: Based on ideas of Osborn et al. 2015, p.2108)
The new care model would enable local primary care systems to test, refine new ideas and make desired changes (Osborn et al. 2015). In context to the above mentioned figure, it can be mentioned that these 10 areas would be covered and emphasized with an aim to improve care and efficiency of existing care systems.
Models of care
A model of care is considered to be a multifaceted concept that defines way by which Healthcare services can be delivered. Also, this model is beneficial in outlining best practices of care delivery through the application of service principles across several clinical streams (Coventry et al. 2015). Models of care are mainly patient-centred and promote equality of Health Services. it is also believed that with these models, stakeholders can influence future policy development in terms of enhanced quality of care, infrastructure and workforce. For instance, the Dementia assessment and improvement framework, a type of care model supports NHS service providers to deliver “outstanding” care to individual suffering from dementia in a community and acute setting. This model of care is based on national policy, practice guidance and resources including the Alzheimer’s Society and HealthWatch 2017. On the other hand, the “Enhanced health in care homes vanguards” model or EHCH care model tends to improve quality of life, health planning and healthcare. This model of NHS England is used for people residing in Connecting Care of Wakefield District, East and North Hertfordshire Clinical Commissioning Group, Nottingham City Clinical Commissioning Group and Newcastle and Gateshead Clinical Commissioning Group.
Development of a new care model for cost reduction and quality improvement
Prior to development of any new model of care, it is essential to ensure that the target community is well invested in the service design. in accordance with the ideas of Sweeney (2017), active engagement and feedback session with Healthcare professionals can help in determining needs of the entire spectrum of primary care. Quality improvement of any care service especially holistic primary care requires focusing on the care users rather than treating them. Therefore, while developing a new care model, active listening can assure time as well as required resources are not wasted. The Models of Care Portal, created by the Southwest Academic Health Science Network (SWAHSN) has provided with relevant resources to aid the process of learning in Primary Health Care. This model also suggests use of primary care resilience tools like Health Education England (HEE) Star Tool and Workflows Analysis Tool (WAT). This care model is an interactive map for the healthcare service providers wish contributes towards Sustainability and Transformation Partnership (STP) areas (Modelsofcare.co.uk, 2019).
Implementation of the new care model
Implementation of such a care model requires radical redesign such that extended care team members and administrative support can be ensured. For this, electronic health record (EHR) becomes essential. However, Litchfield et al. (2015) argued that use of this technological innovation can overburden the professionals as well as the implementation process thereby increasing complexity. As a result of this, medical professionals along with practical nurses need to be empowered beforehand such that they can take the responsibility of completing EHR works. After implementation of the EHCH care model, NHS England has taken initiative to spread this model such that growing complexity of need of underserved population can be addressed. Osborn et al. (2015) added that the NHS Five Year Forward has determined “triple aim” by which improved health and wellbeing, transformed care quality along with sustainable finances can be addressed by 2020.
Discussion of board interaction
Questions to others students of the discussion board
- Do you think that existing models of care of NHS are effective in terms of expense and quality of care?
- What are your recommendations on how to overcome these gaps in the new care model?
Response of questions of two students
- As per your opinion, what are the gaps in existing care models that you will be taking care of in the new model?
I analysed that the cost of entire range of primary care nursing of NHS is increasing at a rapid rate due to implementation of innovative intervention processes and technologies. Use and maintenance of electronic Healthcare record in the form of database is one such reason.
- What are the project constraints that you witnessed while doing this project so far?
Collection and gathering in-depth knowledge on existing care services, models of care and requirement of complying with relevant legislation is time consuming. This further requires access to authentic resources which relies on funding allocated for the project. These factors proved to be some of the major constraints of this project.
(Refer to appendix 1)
Assignment 1B: Project Problem Statement
Problem statement of the project
Social and Healthcare professionals play a vital role in integrated care teams. Technological advancement and innovative methods of intervention have furthermore, allowed these professionals to support individual living with multiple long-term conditions. It also becomes their responsibility to promote and support ownership and independence such that need for residential care packages can be reduced. Along with this cost or expense of availing long-term community support needs to be minimal (De La Torre-Díezet al. 2015). However, the real life scenario is somewhat different. This is evident from the fact that current care models of UK Healthcare provision are mostly ineffective and unsustainable. For instance, expenditure of NHS has been observed to be rising at the rate of 3.7% every year. Technological innovation and implementation of advanced drug and intervention techniques are two most significant reasons behind this.
In spite of this implementation, prevalence of diseases and impact of chronic disability are however increasing. This situation also laid to poor social and healthcare integration which tended hospital beds to be blocked by individuals not requiring hospitalization thereby indicating deteriorated or poor quality of care. Estimations have shown that if this continues, then the ability to spread funds would fall below 1% by 2020 (Montgomery et al. 2017). Internal market modification besides efficiency savings are no more the solution for overcoming these challenges. Number of people suffering from multiple long-term conditions has been witnessed to be increasing from 1.9 million to 2.9 million as of 2018. In between 2014 and 2015, the Department of Health has underspend its budget by 0.001% which in 2016, became overspend (£149 million). Keeping these circumstances into account, it can be mentioned that existing primary care services “improving efficiency” of NHS is not sufficient. Moreover, based on the ideas of Langford et al. (2016), local solutions and long-term intervention and prevention techniques are poorly evaluated.
Main goal behind this project is to develop a new care model for NHS that would help it to reduce cost of intervention and prevention techniques without compromising the quality of care. With this model, this Healthcare organisation would furthermore, be able to invest more in workforce development at all levels. This in turn, would ensure that all Healthcare professionals have adequate knowledge to help and support care seekers to deal with multiple long-term conditions.
Complexity in any healthcare systems indicates presence of inherent messiness and unpredictability. In order to ensure simple yet effective Healthcare services for the target population and community, reduction or avoidance of these complexities needs to be taken into consideration. Therefore, in this project, a new model of care that is free from complexities would be developed as well as implemented. The new care model to be implemented would focus on a specific population and involve primary care from the start. Moreover, it is assumed that with the help of this model, primary care, hospitals and community-based services can be coordinated. In order to ensure that this new model of care is used by collaboration of core, extended care team members, and significant administration, radical redesign of the model would be supported. Also, the model needs to be such that reduces inequality and complies with the up-to-date statement of NHS accountability (Matthews et al. 2016). It has been observed that in UK, budget and strategic policies like Health and Social Care Act 2012 are set by the Department of Health to promote comprehensive health service. Therefore, this model would suggest and assist in complying with these standards.
|
Specific |
To determine components with the help of which an effective primary care model can be ensured for primary health care |
|
Measurable |
Coordination with local overreaching programs such that pitfalls of existing care systems can be avoided |
|
Achievable |
This can be achieved by interviewing a number of Healthcare professionals |
|
Realistic |
With the help of this, “disease detection and treatment” service of NHS can be enhanced |
|
Timeframe |
2 months |
|
Specific |
To critically analyse a number of previously used and existing primary care models |
|
Measurable |
Difficulties in development and implementation would be determined thereby proving to be helpful in reducing complexity of local primary Healthcare systems |
|
Achievable |
In order to achieve this, previous literature and consideration of real-time care models would be critically reviewed |
|
Realistic |
This objective is realistic as with this, real-world gaps in care models can be identified and accordingly would be used for implementation of a new model of care |
|
Timeframe |
3 months |
|
Specific |
To recommend with ways by which the new care model can be implemented in the existing care service of NHS |
|
Measurable |
This objective can be measurable when NHS would able to contribute towards governance accountability, empower its care users and redesign its existing workforce |
|
Achievable |
Focus would be given on initiating change and developing plans for this implementation procedure |
|
Realistic |
This new care model is expected to help NHS to expand its existing service and coverage areas by 50% |
|
Timeframe |
20 days |
Expected outputs of implementation of a new model of care for NHS are as follows:
- This model would help NHS to bring expertise personnel and Healthcare professionals together in order to contributes towards care quality improvement, effective project management, communication and data analysis
- Thorough testing of how intervention techniques will achieve desired level of result can be made possible
- Support can be provided to the local leaders who give their effort in improving existing systems of care
- Decision making roles would be distributed with an aim to plan for changes
- Investment in workforce development would be ensured.
Coventry, P., Lovell, K., Dickens, C., Bower, P., Chew-Graham, C., McElvenny, D., Hann, M., Cherrington, A., Garrett, C., Gibbons, C.J. and Baguley, C., (2015). Integrated primary care for patients with mental and physical multimorbidity: cluster randomised controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. bmj, 350, p.h638.
De La Torre-Díez, I., López-Coronado, M., Vaca, C., Aguado, J.S. and de Castro, C., (2015). Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemedicine and e-Health, 21(2), pp.81-85.
Jones, L., Candy, B., Davis, S., Elliott, M., Gola, A., Harrington, J., Kupeli, N., Lord, K., Moore, K., Scott, S. and Vickerstaff, V., (2016). Development of a model for integrated care at the end of life in advanced dementia: a whole systems UK-wide approach. Palliative medicine, 30(3), pp.279-295.
Langford, M., Higgs, G. and Fry, R., (2016).Multi-modal two-step floating catchment area analysis of primary health care accessibility. Health & place, 38, pp.70-81.
Litchfield, I., Bentham, L., Hill, A., McManus, R.J., Lilford, R. and Greenfield, S., (2015). Routine failures in the process for blood testing and the communication of results to patients in primary care in the UK: a qualitative exploration of patient and provider perspectives. BMJ QualSaf, 24(11), pp.681-690.
Matthews, A., Herrett, E., Gasparrini, A., Van Staa, T., Goldacre, B., Smeeth, L. and Bhaskaran, K., (2016). Impact of statin related media coverage on use of statins: interrupted time series analysis with UK primary care data. bmj, 353, p.i3283.
Modelsofcare.co.uk. (2019).Models of Care Portal. Available at: https://modelsofcare.co.uk/casestudy [Accessed on 12 February 2019]
Montgomery, H.E., Haines, A., Marlow, N., Pearson, G., Mythen, M.G., Grocott, M.P.W. and Swanton, C., (2017). The future of UK healthcare: problems and potential solutions to a system in crisis. Annals of Oncology, 28(8), pp.1751-1755.
Osborn, R., Moulds, D., Schneider, E.C., Doty, M.M., Squires, D. and Sarnak, D.O., (2015). Primary care physicians in ten countries report challenges caring for patients with complex health needs. Health Affairs, 34(12), pp.2104-2112.
Sweeney, K., (2017). Complexity in primary care: understanding its value. Florida, United States: CRC Press.
|
Activities |
Week 1 to 3 |
Week 4 to 6 |
Week 7 to 9 |
Week 10 to 13 |
|
Identifying gaps in exiting models of care |
✓ |
|
|
|
|
Determining project objectives |
✓ |
|
|
|
|
Critical review of literature |
|
✓ |
|
|
|
Planning for a new model of care based on gaps of previous primary health care system |
|
|
✓ |
✓ |
|
Interaction with the Discussion board |
|
|
|
✓ |
